When was the last time you felt truly satiated? Not stuffed to the brim, but simply comfortable and content. That may sound simple, but satiety is an incredibly complex sensation, and can be difficult for some people to experience.
We can think of satiety as having three key components, which work together in a tightly regulated feedback loop:
- The physical sensation of fullness,
- hormonal signaling of nutrient adequacy, and
- sufficient detection and interpretation of these physical and chemical signals in the brain.
In the case of the inflammatory condition known as metabolic syndrome, the balance across these complex feedback loops is lost… but can be restored with a little help.
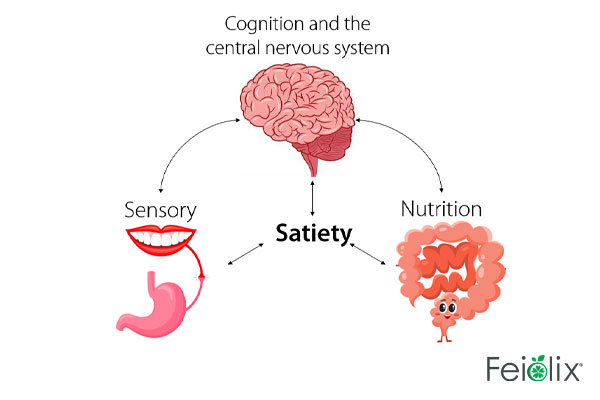
Until recently, satiety was almost exclusively thought of as a physical sensation. Countless products have been developed to increase the sensation of fullness or mimic tastes and textures that we crave without increasing calories. Enter non-digestible bulking fibres, non-caloric sweeteners, and emulsifiers. However, it’s become increasingly clear that the physical aspect of satiety is only one piece of the puzzle, albeit an important piece.
Critically, some of the products developed to mimic flavors and textures and bulk, don’t necessarily register as satiating in our bodies. Our intestines are smarter than we give them credit for and not so easily tricked. Natural fibres, omega-3 fats, and the amino acid glutamate are the primary nutrients detected by chemosensory receptors in the gut, which convert extracellular signals to intracellular responses. Adequate concentrations of nutrients trigger the release of hormones and satiety signals to the vagus nerve and on to the brain, along the gut-brain-axis (Burman 2021).
The activity of chemosensory receptors can be changed with other molecules present in the diet or produced by microbes residing in the gut. For instance, the short chain fatty acid propionate, which is produced by several probiotic species of bacteria utilizing dietary fibre from plants, acts on chemosensory receptors and increases the satiety signals sent to the brain.
GLP-1 – A Potent Signaling Hormone of Satiety
Signals from the chemosensory receptors aren’t the only hunger and satiety signals moving upwards to the brain; hormones and peptides also get in on the action. Leptin, Ghrelin, Peptide YY (PYY), Cholecystokinin (CCK), Glucagon Like Peptide 1( GLP-1), and Insulin are the major players, but there are also minor players that collectively have a large impact across the enteroendocrine and endocrine systems.
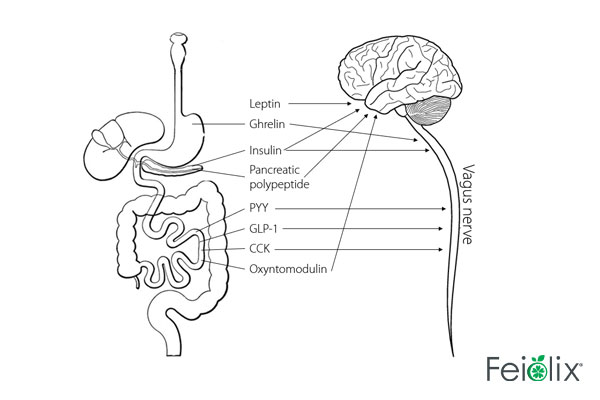
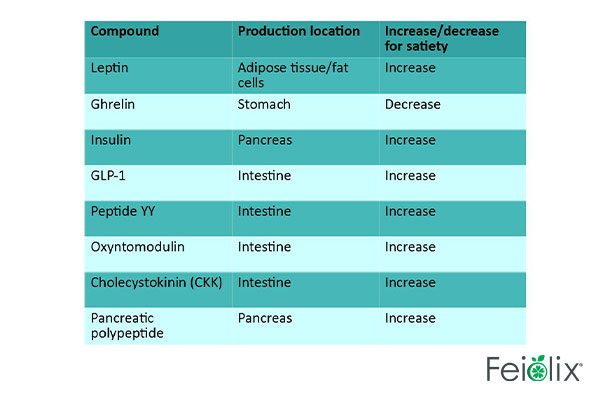
GLP-1 is one of the most potent signaling hormones of satiety and has anti-inflammatory action throughout the body, which makes it one of the most promising targets for treating systemic metabolic disease. GLP-1 has three major benefits:
- Promotes satiety,
- promotes sugar utilization (reducing blood sugar levels), and
- reduces inflammation that is mediated by NFκB, as is characteristic of rheumatoid arthritis, atherosclerosis, type 2 diabetes, and metabolic syndrome (Brierley 2021).
GLP-1 production can be increased by consuming maté, and fruits containing high concentrations of abscisic acid, such as feijoa and figs.
Neuroinflammation – A Possible Cause of Metabolic Syndrome
Getting nutrients right, hosting a thriving gut microbiome, and supporting hormone production and reception are key to achieving satiety. But the experience of satiety as we perceive it is actually occurring in the brain. Just like any other tissue in the body, the brain and central nervous system can become inflamed. Acute inflammation in the brain as an immune response to pathogenic infections (encephalitis) can be life threatening. But sub-acute and chronic inflammation of specific regions of the brain (neuroinflammation) is more common, and while not necessarily life threatening, certainly impacts quality of life and is a predictable consequence of and contributing factor to metabolic syndrome (Purkayastha 2013).
The hypothalamus is the primary region of the brain that acts as the master regulator of energy balance, metabolism, and metabolic syndrome (Myers 2012). Many neurons from the vagus nerve connect directly into the brainstem and the hypothalamus, conveying signals of satiety from the gut.
Crucially, many hormones are able to cross the blood brain barrier and act directly on neurons. Insulin is one such hormone that is transported across the blood brain barrier and acts directly on the hypothalamus (Hampl 2015). A prominent feature of neuroinflammation is insulin resistance in the hypothalamus. Knowing these mechanisms opens up possibilities to address the problem by re-establishing insulin sensitivity.
Luckily, inflammation of the central nervous system responds to specific anti-inflammatory phytochemicals and phytohormones that can be consumed in the diet. Many plant bioactive compounds inhibit the translocation of pro-inflammatory NFκB and subsequent production of inflammatory cytokines and reactive oxygen species, thus reducing neuroinflammation as well as inflammation of many tissues throughout the body and re-establishing insulin sensitivity. Recently it’s been shown that abscisic acid is an insulin sensitizer and reduces neuroinflammation while rescuing the expression of insulin receptor substrate that was otherwise impaired by consumption of a high fat diet (Ribes Navarro 2019). Proper insulin signaling in the brain leads to increased satiety (Hallschmid 2012).
Feiolix Promotes GLP-1 and Increases Insulin Sensitivity
It’s clear that achieving satiety is more than just changing how much food we eat. By eating fruits such as feijoas that are high in anti-inflammatory, GLP-1 promoting, and insulin sensitizing phytohormones, as well as propionate promoting dietary fibre, we can support satiety in our brains and bodies.
References
Brierley, D.I., Holt, M.K., Singh, A. et al. Central and peripheral GLP-1 systems independently suppress eating. Nat Metab 3, 258–273 (2021). https://doi.org/10.1038/s42255-021-00344-4
Burman, A., & Kaji, I. (2021). Luminal Chemosensory Cells in the Small Intestine. Nutrients, 13(11), 3712.
Chaudhri, O. B., Salem, V., Murphy, K. G., & Bloom, S. R. (2008). Gastrointestinal satiety signals. Annu. Rev. Physiol., 70, 239-255.\
Hallschmid, M., Higgs, S., Thienel, M., Ott, V., & Lehnert, H. (2012). Postprandial Administration of Intranasal Insulin Intensifies Satiety and Reduces Intake of Palatable Snacks in Women. Diabetes, 61 (4) 782-789; DOI: 10.2337/db11-1390
Hampl, R., Bičíková, M., & Sosvorová, L. (2015). Hormones and the blood-brain barrier. Hormone molecular biology and clinical investigation, 21(3), 159–164. https://doi.org/10.1515/hmbci-2014-0042
Moran, A. W., Daly, K., Al-Rammahi, M. A., & Shirazi-Beechey, S. P. (2021). Nutrient sensing of gut luminal environment. The Proceedings of the Nutrition Society, 80(1), 29–36. https://doi.org/10.1017/S0029665120007120
Myers, M., Olson, D. Central nervous system control of metabolism. Nature 491, 357–363 (2012). https://doi.org/10.1038/nature11705
Purkayastha, S., & Cai, D. (2013). Neuroinflammatory basis of metabolic syndrome. Molecular metabolism, 2(4), 356-363.
Ribes-Navarro, A., Atef, M., Sánchez-Sarasúa, S., Beltrán-Bretones, M. T., Olucha-Bordonau, F., & Sánchez-Pérez, A. M. (2019). Abscisic acid supplementation rescues high fat diet-induced alterations in hippocampal inflammation and IRSs expression. Molecular neurobiology, 56(1), 454-464.