Feiolix supports healthy blood lipid profiles
Blood sugar tends to take centre stage in Type II diabetes mellitus (T2DM) and Metabolic Syndrome, earning itself quite a reputation for dramatic highs and lows and being difficult to manage. But there’s a whole cast and crew of fats and lipid molecules around those dastardly sugar molecules that play major roles in health dramas as well.
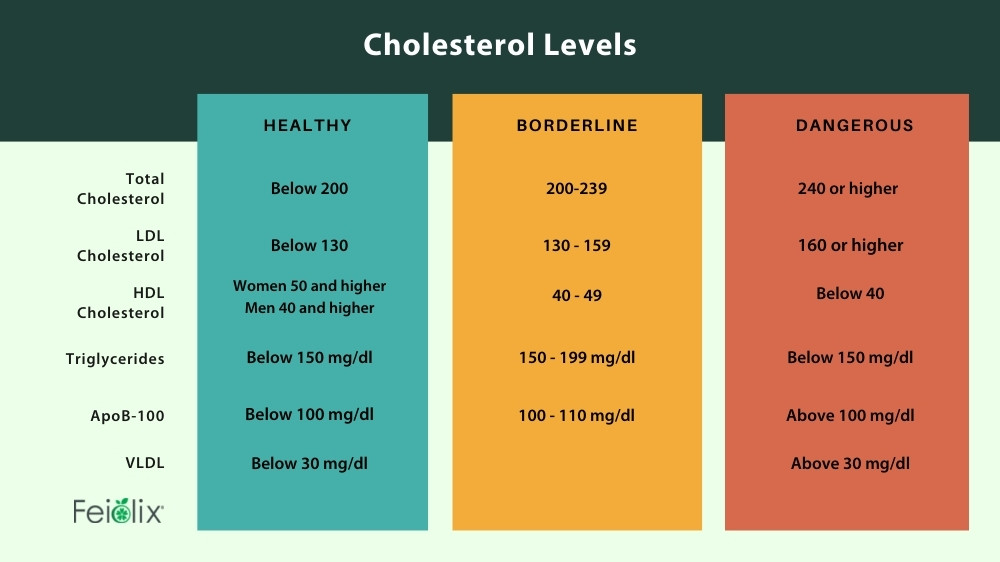
The relevance of fat metabolism to metabolic health isn’t just in body size and shape, although that can be important as well if visceral fat accumulates around vital organs in the abdomen. Abnormalities in lipid metabolism are clearly identified in the 3/5 of the diagnostic criteria for Metabolic Syndrome relating to blood triglycerides, HDL cholesterol, and LDL cholesterol. This overlaps with the estimated 72-85% of T2DM patients who also have diabetic dyslipidaemia, which is associated with substantially increased risk for cardiovascular disease and non-alcoholic fatty liver disease (NAFLD).
It’s been suggested that the dislipidaemia seen in diabetics and metabolic syndrome is due to lifestyle factors such as a high fat diet, but there’s much more going on in terms of how fats are metabolised and the quality and storage of the molecules resulting from that metabolism. The common connection here between dislipidaemia, diabetes and metabolic syndrome is insulin which is the primary director of energy utilisation and metabolism: supporting insulin sensitivity can pull both blood sugar and blood lipids back into balance.
Insulin has two primary effects on lipid metabolism:
- Insulin promotes the conversion of free fatty acids to lipoproteins in the liver when the liver is saturated with glycogen. These lipoproteins are then exported back into the blood stream for further utilisation or accumulation.
- Insulin inhibits the breakdown of triglycerides into free fatty acids in adipose tissue by inhibiting lipase, leading to accumulation of fat.
But this isn’t just a one-way street, free fatty acids in the blood also cause insulin resistance in muscle cells by inhibiting insulin-stimulated glucose absorption and glycogen synthesis. Insulin resistance means that cells don’t absorb glucose from the blood stream quickly enough when insulin is released from the pancreas. This leaves both glucose and insulin circulating in the blood which can be dangerous for nerves and the kidneys.
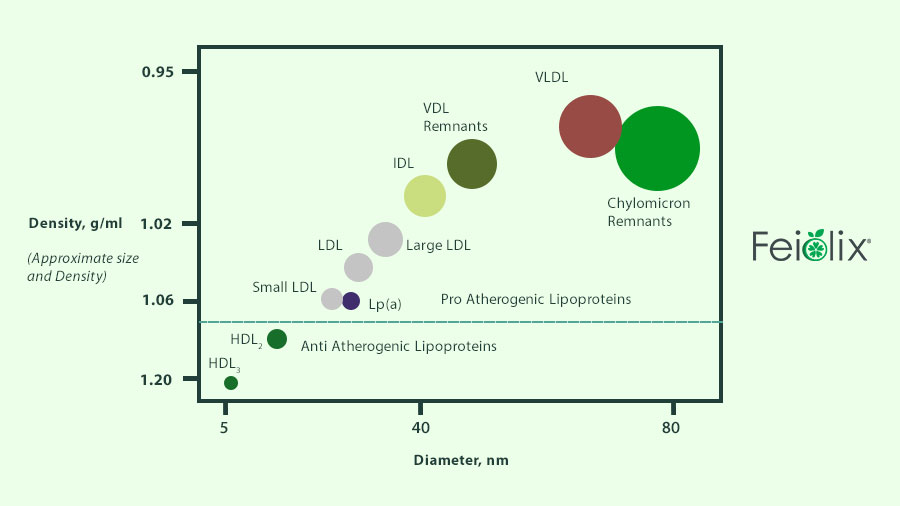
Circulating glucose and free fatty acids eventually arrive at the liver. When the liver is presented with excessive fatty acids and insulin, dangerous and atherosclerotic LDL and VLDL cholesterols are produced. This process is controlled by ApoB, often considered the gate keeper to danger. Diets high in sugar and fat promote ApoB production. As more ApoB is produced, more free fatty acids are converted into LDL and VLDL, which tend to stick to the inside walls of arteries, leading to atherosclerosis.
HDL is termed the good cholesterol because it’s atheroprotective and functions in reverse cholesterol transport: the movement of cholesterol away from peripheral cells and arteries to the liver from catabolism and excretion. HDL contains a lipoprotein called ApoA-1 which is at the core of this action, making it the gatekeeper to health. Doctors are increasingly looking at the ratio of Apo-B/ApoA-1 to measure a patient’s risk of heart attack.
It’s important to note that everyone has a specific and unique metabolic phenotype, especially when it comes to lipid metabolism. Some people carry genes to produce more ApoB, which increases their risk for cardiovascular disease, whereas other people can consume the same diet and lead a similar lifestyle with no ill-effects on their metabolic health. It is still important to maintain insulin sensitivity, and there are many changes we can make to reduce insulin resistance.
Things we can do to reduce insulin resistance and improve insulin sensitivity:
- Nutrition: managing macronutrient ratios and energy consumption is the first line of defence against insulin resistance.
- Sleep: getting at least 7 hours of high-quality sleep with multiple REM cycles is critical for maintaining insulin sensitivity. Sleep deprivation lasting more than 24 hours seems to impair pancreatic B cell function.
- Exercise: both cardio and resistance exercise (anaerobic and aerobic) help promote glucose absorption and utilisation in the short term. Over the long term, expression of GLUT4 transporters for the uptake of glucose into cells is also increased, improving insulin sensitivity even on off days.
- Plant bioactives: Some secondary metabolites and hormones produced in plants have potent insulin sensitising actions.
Feiolix contains multiple bioactives that improve insulin sensitivity and dislipidaemia associated with metabolic syndrome.
Abscisic acid and polyphenols found in Feiolix both promote the browning of white fat, meaning the addition of energy utilising mitochondria to otherwise low energy utilising white adipose cells. Abscisic acid and polyphenols also promote energy usage (thermogenesis) in brown adipose tissue, meaning more free fatty acids and glucose is absorbed and burned, particularly right after a meal. Abscisic acid also stimulates glucose absorption and reduces the need for higher levels of insulin to be secreted from the pancreas. This in turn reduces the production of dangerous LDL and VLDL molecules in the liver. Polyphenols have been found to increase the reverse transport of cholesterol by HDL and ApoA-1, which helps to reduce LDL and VLDL and protect patients from CVD and more serious events.
By maintaining a healthy lifestyle, eating a polyphenol rich diet, and supplementing diet with potent bioactive compounds such as those found in Feiolix, it’s possible to improve your blood lipid profile along with overall metabolic health.
Glossary
Free fatty acids: lipid species released from the adipose tissue and several cell types upon lipolysis. Apart from their classical roles in energy supply or as structural components, FFAs are active players in many biological processes.
Triglycerides: are lipids derived from glycerol and three fatty acids.
Glycogen: is a multi-branched polysaccharide of glucose that stores energy.
Lipoproteins: are structures containing both protein and fat that carry cholesterol through the bloodstream.
Cholesterol: is a sterol, which is a type of lipid. Cholesterols are crucial structural and functional components of healthy cells, but too much cholesterol can increase risk of heart disease.
Chylomicrons: Large triglyceride rich particles made by the intestine to transport dietary triglcyerides and cholesterol to peripheral tissues and the liver. The size of the chylomicron depends on the amount of fat ingested, but each chylomicron contain several apolipoproteins, as well as a core structural Apo B-48 molecule.
Chylomicron remnants: As peripheral tissues remove triglycerides from chylomicrons, smaller chylomicron remnants are formed, which are pro-atherogenic.
HDL High density lipoprotein: HDL, or “good” cholesterol, absorbs cholesterol and carries it back to the liver. The liver then flushes it from the body. High levels of HDL cholesterol can lower your risk for heart disease and stroke (anti-atherogenic).
IDL: Intermediate density lipoproteins, which are proatherogenic, result from the removal of triglycerides from VLDL
LDL small dense low density lipoprotein cholesterol LDL, sometimes called “bad” cholesterol, makes up most of your body’s cholesterol. High levels of LDL cholesterol raise your risk for heart disease and stroke (pro-atherogenic). LDL particles exist in multiple subclasses which vary by size, density, and lipid content.
VLDL very low-density lipoprotein cholesterol are large and contain the highest amount of triglycerides. High levels of VLDL can contribute to atherosclerosis, which can make a person more susceptible to heart disease or stroke. Eating more carbohydrates, or sugars, than you burn can lead to excessive amounts of triglycerides and high levels of VLDL in your blood.
ApoB-100: Apolipoprotein B-100 is a type of VLDL and allows LDLs to attach to specific receptors on the surface of cells, particularly in the liver. Once attached, the receptors transport LDLs into the cell, where they are broken down to release cholesterol. Elevated levels of apo B correspond to elevated levels of LDL-C and to non-HDL-C and are associated with an increased risk of cardiovascular disease (CVD). Elevations may be due to a high-fat diet and/or decreased clearing of LDL from the blood.
ApoA-1: Apolipoprotein A1 is a major component of HDL particles. ApoA-1 enables efflux of fat molecules from within peripheral cells (arteries and macrophages) for transport to the liver for catabolism and excretion.
White adipose tissue collects, stores and then releases lipids. White adipose tissue is increasingly recognised an endocrine organ, as it also releases leptin (a satiety hormone), inflammatory cytokines, and molecules that participate in lipid metabolism vascular haemostasis (bleeding).
Brown adipose tissue is an energy utiliser and essential in generating heat. Brown adipose tissue contains more mitochondria than white adipose tissue.
References:
Advances Protein Chemistry 45:303, 1994
Athyros, V.G., Doumas, M., Imprialos, K.P. et al. Diabetes and lipid metabolism. Hormones 17, 61–67 (2018). https://doi.org/10.1007/s42000-018-0014-8
Boden G. (1999). Free fatty acids, insulin resistance, and type 2 diabetes mellitus. Proceedings of the Association of American Physicians, 111(3), 241–248. https://doi.org/10.1046/j.1525-1381.1999.99220.x
Brunzell, J. D., & Ayyobi, A. F. (2003). Dyslipidemia in the metabolic syndrome and type 2 diabetes mellitus. The American journal of medicine, 115 Suppl 8A, 24S–28S. https://doi.org/10.1016/j.amjmed.2003.08.011
Chen, L., Chen, X. W., Huang, X., Song, B. L., Wang, Y., & Wang, Y. (2019). Regulation of glucose and lipid metabolism in health and disease. Science China. Life sciences, 62(11), 1420–1458. https://doi.org/10.1007/s11427-019-1563-3
Feingold KR. Introduction to Lipids and Lipoproteins. [Updated 2021 Jan 19]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK305896/
Matacchione, G., Gurău, F., Baldoni, S., Prattichizzo, F., Silvestrini, A., Giuliani, A., … & Sabbatinelli, J. (2020). Pleiotropic effects of polyphenols on glucose and lipid metabolism: Focus on clinical trials. Ageing Research Reviews, 61, 101074.
Millar, C. L., Duclos, Q., & Blesso, C. N. (2017). Effects of Dietary Flavonoids on Reverse Cholesterol Transport, HDL Metabolism, and HDL Function. Advances in nutrition (Bethesda, Md.), 8(2), 226–239. https://doi.org/10.3945/an.116.014050
Parhofer K. G. (2015). Interaction between Glucose and Lipid Metabolism: More than Diabetic Dyslipidemia. Diabetes & metabolism journal, 39(5), 353–362. https://doi.org/10.4093/dmj.2015.39.5.353